Neurodegenerative diseases are a group of chronic, progressive disorders characterized by the degeneration of neurons in the brain and/or spinal cord, resulting in a gradual loss of cognitive, motor, and sensory functions. These diseases include Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and amyotrophic lateral sclerosis (ALS). Despite intensive research efforts, there are currently no effective treatments that can reverse or halt the progression of these diseases.
Stem cell therapy has emerged as a promising therapeutic approach for neurodegenerative diseases, as it offers the potential to replace lost or damaged cells and promote tissue repair and regeneration. This review will provide an overview of the current state of research on stem cell therapy for neurodegenerative diseases, including the types of stem cells used, the mechanisms of action, and the clinical applications and challenges.
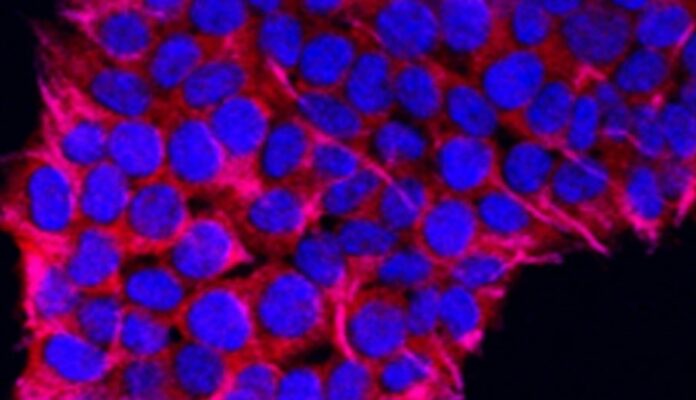
Stem cells are undifferentiated cells that have the ability to differentiate into various cell types and self-renew. They can be classified into two broad categories: embryonic stem cells (ESCs) and adult stem cells.
ESCs are derived from the inner cell mass of a developing embryo and have the potential to differentiate into any cell type in the body. However, their use in clinical applications is limited due to ethical and regulatory concerns and the risk of tumor formation.
Adult stem cells are found in various tissues and organs throughout the body and are responsible for tissue maintenance and repair. They can be further classified based on their origin and differentiation potential. For example, hematopoietic stem cells (HSCs) are found in the bone marrow and can differentiate into all blood cell types, while mesenchymal stem cells (MSCs) are found in the bone marrow, adipose tissue, and other organs and can differentiate into various cell types, including bone, cartilage, and fat cells.
In addition to ESCs and adult stem cells, induced pluripotent stem cells (iPSCs) have also emerged as a promising source of stem cells for therapeutic applications. iPSCs are generated by reprogramming adult cells, such as skin cells, into an embryonic-like state, thereby obtaining the ability to differentiate into any cell type in the body.
Stem cell therapy for neurodegenerative diseases can work through several mechanisms, including cell replacement, neuroprotection, and immunomodulation.
The most straightforward approach to stem cell therapy is to replace the lost or damaged cells with healthy cells. For example, in Parkinson’s disease, dopaminergic neurons in the substantia nigra are gradually lost, resulting in the characteristic motor symptoms. Stem cell therapy aims to replace these lost neurons with new, functional ones.
Several studies have demonstrated the potential of stem cells to differentiate into dopaminergic neurons and improve motor function in animal models of Parkinson’s disease. For example, a study by Grealish et al. (2014) showed that transplantation of human ESC-derived dopaminergic neurons into the striatum of Parkinsonian rats led to significant improvements in motor behavior and increased dopamine release.
Stem cells can also exert neuroprotective effects by promoting the survival and function of existing neurons. For example, MSCs have been shown to secrete various neurotrophic factors, such as brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF), which can promote neuronal survival and regeneration.
In addition, stem cells can also modulate the immune response and reduce inflammation, which is a common feature of neurodegenerative diseases. For example, a study by Cui et al. (2013) showed that transplantation of MSCs into the spinal cord of ALS mice led to a reduction in microglial activation and pro-inflammatory cytokine response levels, as well as an increase in anti-inflammatory cytokines, resulting in improved motor function and survival.
Neurodegenerative diseases are often associated with chronic inflammation and immune dysfunction. Stem cells can modulate the immune response by promoting the expansion of regulatory T cells and reducing the activity of pro-inflammatory immune cells, such as microglia.
For example, a study by Zhao et al. (2017) showed that transplantation of human umbilical cord MSCs into the brain of Alzheimer’s disease mice led to a reduction in amyloid-beta deposition, microglial activation, and pro-inflammatory cytokine levels, as well as an increase in anti-inflammatory cytokines and synaptic markers, resulting in improved cognitive function.
Stem cell therapy for neurodegenerative diseases is still in the early stages of development and is mainly being studied in preclinical animal models and early-phase clinical trials. However, several promising studies have demonstrated the potential of stem cell therapy for the treatment of neurodegenerative diseases.
Several clinical trials have investigated the safety and efficacy of stem cell therapy for Parkinson’s disease. A phase I/II trial by Mendez et al. (2018) showed that transplantation of autologous MSCs into the striatum of Parkinson’s disease patients was safe and well-tolerated, and led to significant improvements in motor function and quality of life.
Another phase I/II trial by Barker et al. (2018) investigated the safety and efficacy of transplantation of human ESC-derived dopaminergic neurons into the striatum of Parkinson’s disease patients. The study showed that the transplantation was safe and well-tolerated, and led to significant improvements in motor function and quality of life.
Several preclinical studies have demonstrated the potential of stem cell therapy for Alzheimer’s disease. A study by Blurton-Jones et al. (2014) showed that transplantation of human ESC-derived neural progenitor cells into the hippocampus of Alzheimer’s disease mice led to a reduction in amyloid-beta deposition, microglial activation, and neuroinflammation, as well as an improvement in cognitive function.
Another study by Lee et al. (2018) showed that transplantation of human umbilical cord blood-derived MSCs into the brain of Alzheimer’s disease mice led to a reduction in amyloid-beta deposition, tau hyperphosphorylation, and neuroinflammation, as well as an improvement in cognitive function.
Several clinical trials have investigated the safety and efficacy of stem cell therapy for ALS. A phase I/II trial by Mazzini et al. (2015) showed that transplantation of autologous MSCs into the spinal cord of ALS patients was safe and well-tolerated, and led to a reduction in disease progression and improvement in quality of life.
Another phase I/II trial by Glass et al. (2012) investigated the safety and efficacy of transplantation of human ESC-derived motor neurons into the spinal cord of ALS patients. The study showed that the transplantation was safe and well-tolerated, and led to a reduction in disease progression and improvement in motor function.
Despite the promising results of preclinical studies and early-phase clinical trials, stem cell therapy for neurodegenerative diseases still faces several challenges and limitations.
One of the major challenges is the variability and heterogeneity of stem cells, both within and between donors. The quality and potency of stem cells can vary depending on factors such as donor age, health status, and tissue source, as well as the methods of isolation, expansion, and differentiation. Standardization and quality control of stem cell products are therefore crucial for ensuring safety and efficacy.
Another challenge is the potential for tumorigenicity response and teratogenicity, which refers to the potential for stem cells to form tumors or differentiate into unintended cell types, respectively. To mitigate these risks, rigorous preclinical safety testing and long-term monitoring of patients are essential.
In addition, the optimal dosing, timing, and route of administration of stem cells for neurodegenerative diseases are still unclear. Different types of stem cells may require different dosages, frequencies, and delivery methods, depending on the target tissue and disease stage. Further research is needed to optimize the therapeutic protocols and maximize the clinical benefits of stem cell therapy.
Another challenge is the lack of understanding of the underlying mechanisms of stem cell therapy for neurodegenerative diseases. Although several hypotheses have been proposed, the precise mechanisms by which stem cells exert their therapeutic effects are still not fully understood. More research is needed to elucidate the molecular and cellular pathways involved in stem cell-mediated neuroprotection and repair.
Finally, the cost-effectiveness and scalability of stem cell therapy for neurodegenerative diseases are still uncertain. Stem cell therapy is a complex and expensive procedure that requires specialized facilities, skilled personnel, and high-quality equipment. The long-term costs and benefits of stem cell therapy need to be carefully evaluated in comparison to other treatment options, such as pharmacotherapy and rehabilitation.
Despite these challenges, stem cell therapy holds great promise for the treatment of neurodegenerative diseases. With continued research and development, stem cell therapy may become a safe, effective, and accessible treatment option for millions of patients worldwide who are suffering from these devastating disorders.